When you lose an adult tooth, replacing it promptly with the best dentists in Coral Gables is key to protecting your oral health. When there's a hole in your smile, the surrounding teeth will start to shift toward the available space, affecting your bite alignment.
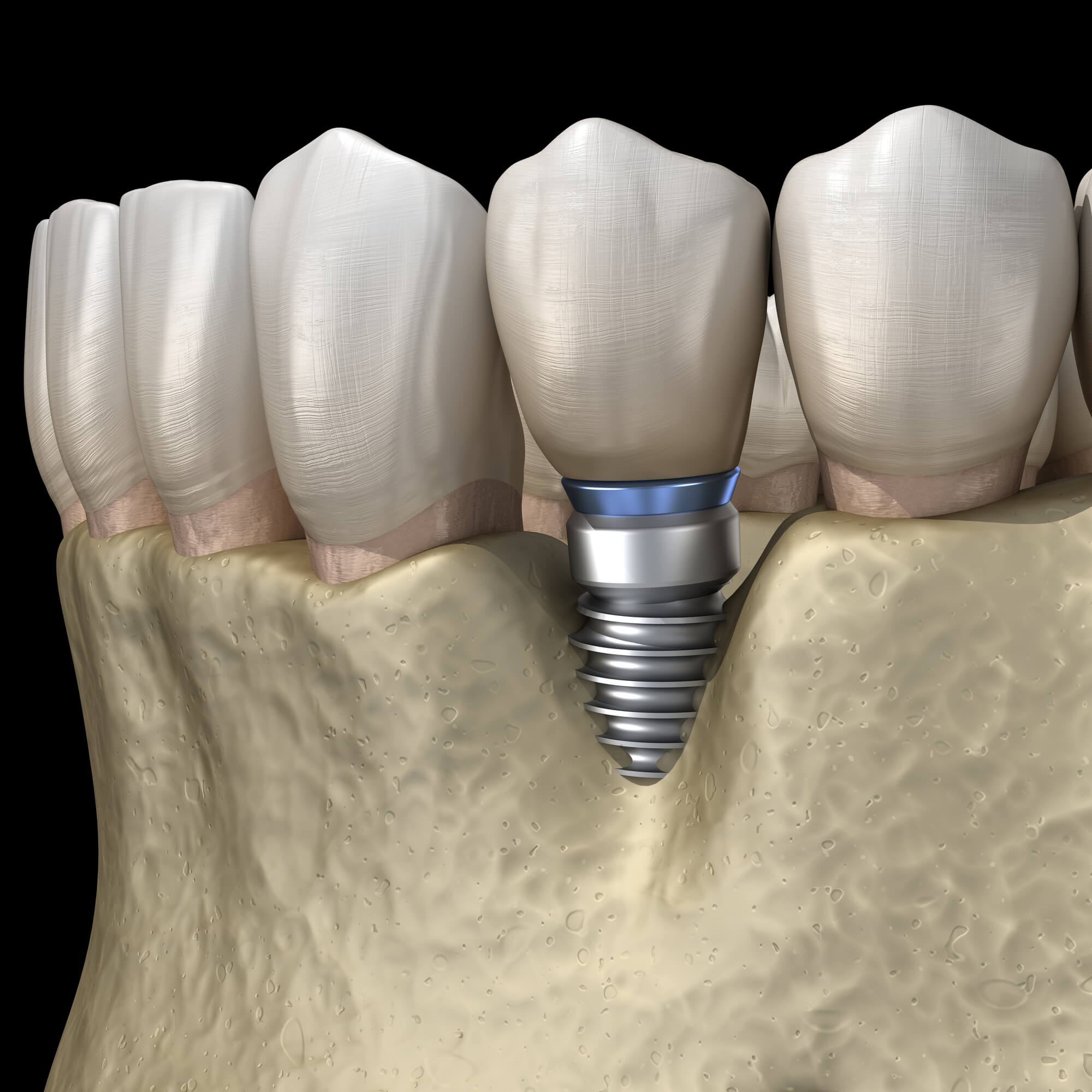
Moreover, missing teeth can lead to bone resorption, a dangerous condition that may foster further tooth loss over time. Replacing teeth with implants is key, and properly taking care of your restorations can prevent infection. Here, we'll explain peri-implantitis and what you can do to avoid it.

Peri-implantitis is a disease that causes inflammation of the soft tissues and bone loss around an osseointegrated implant. In essence, it is a dental emergency similar to gum disease that surrounds an implant site.
If untreated, it may lead to implant failure and bone loss. This condition is not common: in fact, only 5% to 8% of implant patients develop an infection. However, certain factors may increase your risks, such as the health of the surrounding tissue, the implant's design, the degree of roughness, the external morphology, and whether the area suffers excessive mechanical strain through bruxism.
Additionally, certain risk factors increase your chances of developing peri-implantitis, such as:
When identified early, damage caused by peri-implantitis can be repaired, and more severe issues can be avoided, making early detection essential.
Peri-implantitis often starts as an infection in the gums; for that reason, its symptoms are similar to those of gingivitis. This includes changes in gingival color, bleeding, and probing depth of peri-implant pockets. Some signs to look out for in detail include:

Implant failure is often caused by two main factors: bad oral hygiene habits and genetic predispositions. The common causes of this condition include:
The first sign of peri-implantitis is a biofilm that forms around the implant. A biofilm is a complex collection of bacteria enclosed in a protective matrix. The bacteria in this biofilm release toxic substances that lead to inflammation in the surrounding tissues.
The immune system may respond to this inflammation by causing bone loss, which could ultimately lead to implant failure.
Poor dental hygiene is one of the main causes of peri-implantitis. Failing to brush after every meal and not flossing daily can lead to bacterial plaque buildup on the surface of implants and along the gum line.
Eventually, this plaque turns into tartar, which is harder to get rid of. Without treatment, the bacteria that cause tartar and plaque can irritate and infect the tissues around them.
Smoking is a major risk factor for peri-implantitis. Nicotine weakens the body's defenses against infection by reducing the blood flow to the gums. Additionally, smoking may weaken immunity, making it more difficult to combat the bacteria that cause peri-implantitis.
Although the precise role of genetics in peri-implantitis is still unknown, certain people may be at a higher risk of developing the condition. Systemic illnesses like diabetes, osteoporosis, and rheumatoid arthritis that affect the body's immune system and overall health can also raise the risk.
The risk of bacterial infection in the tissue surrounding an implant is increased when implants are positioned incorrectly or in regions with inadequate bone support.
Furthermore, peri-implantitis can result from applying excessive force to the implant from biting or chewing hard foods. This force can accelerate the implant's wear and damage and cause small fissures, giving bacteria a place to hide.
Inadequately fitting crowns or other restorations can irritate and inflame the tissue surrounding the implant, resulting in peri-implantitis.
Following dental implant treatment, your periodontist or dentist will want to schedule at least one follow-up visit with you. During this visit, they will examine the implant and surrounding tissue for any issues. Neglecting your follow-up could let minor issues escalate into more serious ones, fostering peri-implantitis.
As we mentioned, peri-implantitis is often brought on by a lack of proper oral hygiene habits. Therefore, keeping good care habits after implant surgery is key to preventing this condition. Some care tips to incorporate include:
We may explore alternative treatment options depending on whether the bacterial mucosa has already started to build up around the implant site. The main goals of implant infection management are alveolar bone regeneration, infection control, and implant surface cleaning.
Early intervention and rigorous adherence to the recommended treatment plan depend on the longevity of dental implants and the successful treatment of peri-implantitis.
In extreme circumstances where the implant is compromised, it might be required to be removed and replaced.
It is important to maintain proper oral hygiene at home and make an appointment for routine dental checkups and cleanings. Finding early warning indicators of recurrence requires routine implant health monitoring.
Treating peri-implantitis early on is crucial to preventing implant failure and protecting your oral and overall health. Still have questions about this condition? Let’s go over some frequently asked questions!
Peri-implantitis can be exacerbated by smoking, diabetes, poor oral hygiene, and other systemic conditions.
Bad breath, bleeding, red, swollen gums, and pain or discomfort near the implant indicate infection around the implant site.
Options for treatment include nonsurgical techniques like expert cleaning and, in more extreme situations, surgical techniques like bone grafting or implant removal.
Yes, peri-implantitis can be considerably decreased by maintaining proper oral hygiene, getting regular dental exams, and quitting smoking.
Peri-implantitis is most prevalent among people who smoke, with around 20% experiencing implant failure. Other conditions, such as diabetes, or people who have had dental implants for many years, have higher chances of developing this condition, too.

For implants to last long, peri-implantitis must be identified early and treated. Patients and dental professionals need to check the condition of implants regularly.
By staying vigilant and seeking professional care, patients can enjoy the long-term benefits of their dental implants and considerably lower their chance of developing peri-implantitis. If you suspect you may suffer from this condition, Coral Gables Dentistry can help. Contact us today to set an appointment!
We value your time, so we always run on schedule, respecting your commitments, with no double bookings and minimal wait times. Experience dentistry like never before in our award-winning clinic.